The Importance of Routine Psychometric Testing for Mild Cognitive Impairment in Geriatric Populations
Author: VP Grewal, MD. 2020 September 3.
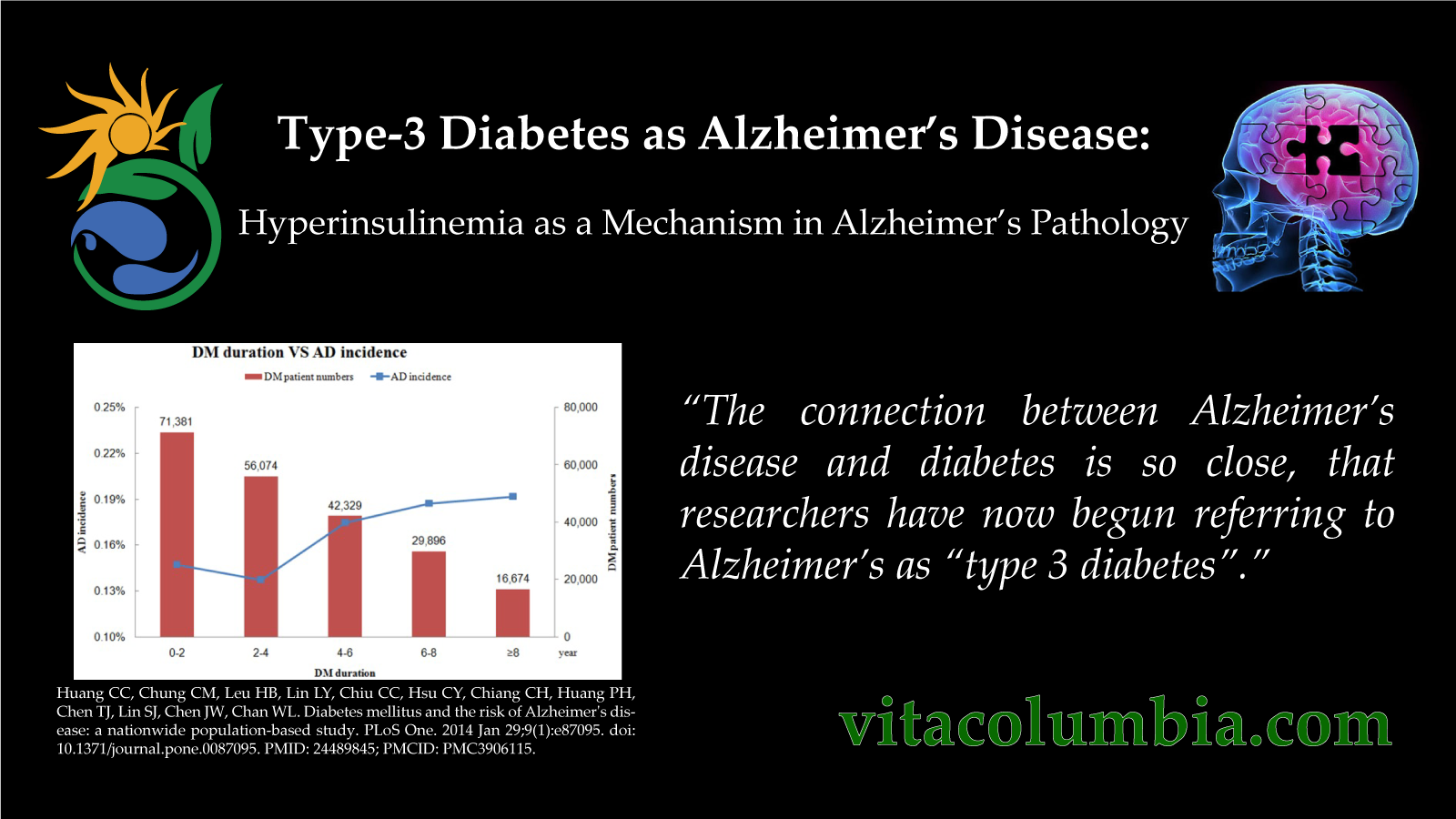
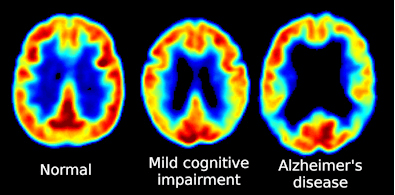
The National Institute on Aging and Alzheimer’s Association (NIA-AA) defines Alzheimer’s Disease (AD) as a progressive disease with three stages, an asymptomatic pre-clinical stage, mild cognitive impairment (MCI), and Alzheimer’s dementia. In AD, there is an accumulation of β-amyloid protein at neuronal synapses, eventually leading to synaptic failure and neuronal death. Intracellularly, tau proteins accumulate which inhibit the transport of nutrients and other essential molecules, hastening the process the cell death. Initially the patient is able to compensate for the neuronal changes and shows no cognitive decline. Eventually, basic bodily functions such as swallowing are impaired. Patients will ultimately become bed-ridden, and will typically die from external factors such as pneumonia and infected pressure ulcers. The time of disease progression is highly variable among individuals.
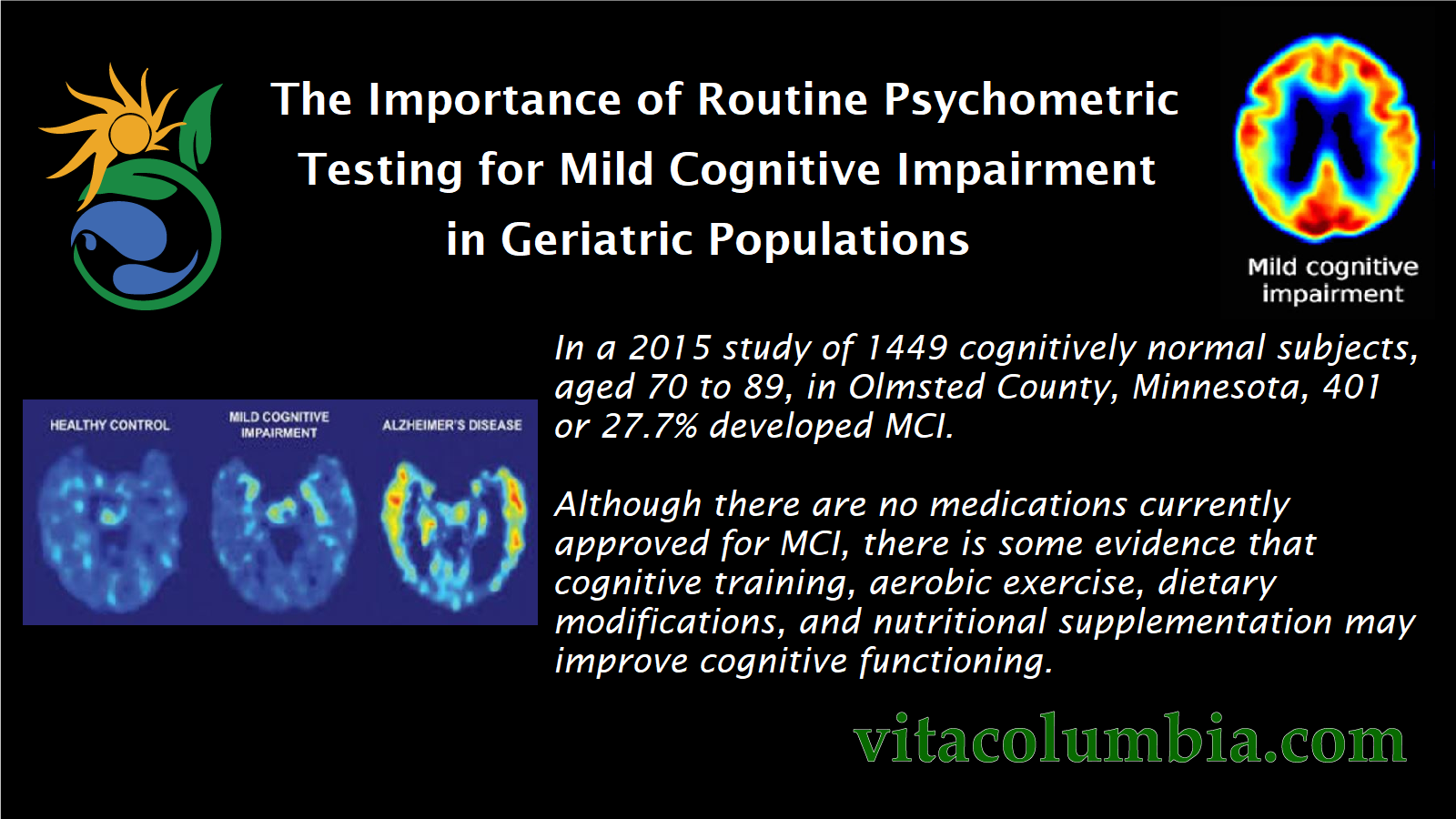
MCI is an intermediate stage between the cognitive decline of normal aging and dementia. MCI will often, but not always, progress to dementia. Causes of MCI include neurodegenerative disease, medications, depression, vascular problems, and other disease processes. The cognitive deficit of MCI may not interfere with a patient’s ability to function independently. Patients will often attribute the subtle symptoms to aging or stress. The revised Mayo Clinic Criteria classifies MCI into two categories, amnestic MCI (a-MCI) and non-amnestic MCI (na-MCI). a-MCI primarily effects episodic memory, and na-MCI primarily effects language, decision-making, judgement, time-perception, or visuospatial abilities. Studies show up to 70% of those with a-MCI will develop Alzheimer’s, while other variants will develop dementia of other causes. The conversion rate from MCI to AD is estimated to be 15% per year. Those who revert back to a normal cognitive state, have an increased risk for entering MCI again, and for developing dementia. In a 2015 study of 1449 cognitively normal subjects, aged 70 to 89, in Olmsted County, Minnesota, 401 or 27.7% developed MCI. Although there are no medications currently approved for MCI, there is some evidence that cognitive training, aerobic exercise, dietary modifications, and nutritional supplementation may improve cognitive functioning.
In the research field, early MCI detection is crucial to study interventions that delay progression. In a clinical setting, early MCI detection is important because it allows physicians to rule out any non-AD causes, consider non-pharmacological intervention, and explore participation in clinical research trials with the patient. Patients and their families also benefit from identification of MCI as they can make future preparations while the patient is in a capable cognitive state.
Assessing the progression from MCI to Alzheimer’s dementia requires routine psychometric assessments. The use of formal psychometric testing by primary care practitioners for diagnosing dementia was estimated to be only 58%, with the main reported barrier being lack of time. Furthermore, commonly employed psychometric tools such as the Alzheimer’s Disease Assessment Scale (ADAS-cog) and Mini-Mental Status Exam (MMSE) are useful in monitoring AD progression, but lack sensitivity for MCI. The Clinical Dementia Rating Scale (CDR) was one of the first assessment tools that showed sensitivity for MCI, assessing daily functional activity, interviewing both patient and a caregiver. Unfortunately, the CDR is primarily subjective and has a long administration time.
The Montreal Cognitive Assessment (MoCA) is a psychometric tool developed by Dr. Z Nasreddine. The scale specifies parameters for normal controls, MCI, and AD, and estimates up to 90% specificity for MCI. Recent date indicates a statistically significant correlation with existing scales in terms of total score and individual parameters. The administration time for the MoCA is less that 10 minutes. It currently does not require any specific training or certification for administration, but does require an expert in the cognitive field to interpret the results. The ease of administration, accuracy, and sensitivity for both MCI and AD allows the MoCA to serve as a routine cognitive assessment by health care providers.
References:
Brooks LG, Loewenstain DA. Assessing the progression of mild cognitive impairment tto Alzheimer’s disease: current trends and future directions. Alzheimers Res Ther 2010, 2:28.
Cherry DL, Vickery BG, Schwankovsky L, Heck E, Plauchm M, Yep R (2004) Interventions to improve quality of care: the KLaiser Permanente-Alzheimer’s Association Dementia Care Project. Am J Manag Care 10: pp 553-560.
Grewal VP. A Comparative Analysis of a Novel Psychometric Tool for Alzheimer’s Dementia with the Modified ADAS-Cog. Mechanisms, Clinical Strategies, and Promising Treatments of Neurodegenerative Diseases. 12th International Conference AD/PD Nice, France, March 18-22, 2015: Abstracts. Neurodegen Dis 2015;15(suppl1): 1117-1118.
Jicha GA, Parisi JE, Dickson DW, Johnson K, Cha R, Ivnik RJ, Tangalos EG, Boeve BF, Knopman DS, Braak H, Petersen RC. Neuropathologic outcome of mild cognitive impairment following progression to clinical dementia. Arach Nerol. 2006 May;63(5):674-81.
Lim WS. Chong MS, Sahadevan S. Review: Utility of the Clinical Dementia Rating in Asian Populations. Clinical Medicine and Research. 2007;5:61-70.
Nasreddine ZS, Phillips NA, Bedirian V, Charbonneau S, Whitehead V, Collin I, Cummings JL, Chertkow H. The Montreal Cognitive Assessment (MoCA): A Brief Screening Tool For Mild Cognitive Impairment.
Petersen RC, Caracciolo B , Brayne C, Gauthier S, Jelic V, Fratiglioni L. Mild cognitive impairment: a concept in evolution (Key Symposium). J Intern Med 2014; 275: 214-228.
Pankatz VS, Roberto RO, Mielke MM, Knopman DS, Jack CR, Geda YE, Rocca WA, Pterson R. Predicting the risk of mild cognitive impairment in the Mayo Clinic Study of Aging. Neurology. April 7, 2015. 84:14. 1433-1442
In a 2015 study of 1449 cognitively normal subjects, aged 70 to 89, in Olmsted County, Minnesota, 401 or 27.7% developed MCI.
Although there are no medications currently approved for MCI, there is some evidence that cognitive training, aerobic exercise, dietary modifications, and nutritional supplementation may improve cognitive functioning.